Most women are unaware they have dense breasts until they reach the age of 45.
Dense breasts, with relatively little fat and more connective and glandular tissue, have the highest risk of cancer. The pattern of these tissues on a mammogram is difficult to distinguish from tumors—dense connective tissue and tumors both appear white against a dark background. Breast density usually decreases with age or body mass index (BMI) and increases with hormone replacement therapy. [1]
An estimated 66 percent of premenopausal women, and 25 percent of postmenopausal women, have breasts that are dense enough to interfere with mammogram accuracy. Studies show that having dense breasts raises the risk of developing breast cancer fourfold to sixfold, primarily because density can obscure tumors. [3,4]
In a study of 329,495 women undergoing screening mammography in the United States between 1996 and 1998, mammography had 24 percent less sensitivity with 8 percent less specificity. [2]
MRI Screening
The potential of MRI for screening women with dense breasts remains controversial due to scant clinical evidence. It is possible that MRI could offer a cost-effective supplemental imaging option for dense-breast women. The goal is earlier detection of small and potentially more-aggressive lesions are missed in mammographically dense breasts.
Dynamic contrast-enhanced (DCE) MRI has the highest reported sensitivity of all diagnostic breast imaging modalities for detecting abnormalities. However, methods of MRI is an expensive option and measurement requires standardization and automation. [5]
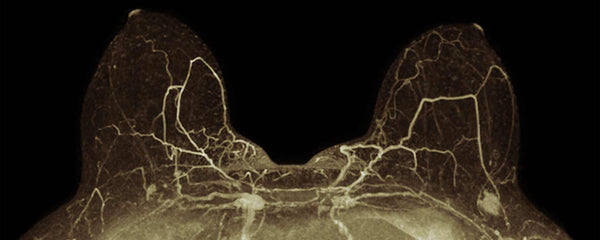
An example of maximum-intensity projection image from a screening MRI demonstrates a suspicious mass in the left breast that was subsequently biopsied and found to be early-stage invasive ductal carcinoma. —Lee C, MD MS, et al. [2]
Ultrasound vs. Mammography
Common concerns among patients include skepticism over accuracy of mammography (breast x-ray) screening. Should you have ultrasound or another supplemental screening? Ultrasound has advantages of not emitting ionizing radiation, being well tolerated by patients, and already being widely available. [2]
Google Health Artificial Intelligence Examines Breasts
🤖 “AI could boost the quality of breast cancer screening in the US and maintain the same level in the UK, with the AI assisting or replacing the second radiologist. The AI outperformed the specialists by detecting cancers that the radiologists missed in the images, while ignoring features they falsely flagged as possible tumours.” —The Guardian
Studies have shown that ultrasound significantly increases detection of clinically important, small, invasive, node-negative cancers within dense breasts. This is because tumors appear dark in contrast to lighter glandular tissue. For orientation of anomalies, ultrasound usually supplements other imaging. [6]
October Breast Cancer Awareness Month
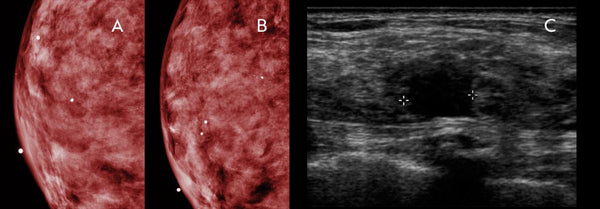
(A, B) Dense tissue obscures breast cancer that is easily visible on ultrasound image. (C) Handheld high-resolution ultrasound reveals a 1.2 cm irregular mass, denoted by calipers in the image, which was subsequently biopsied and proven to be invasive ductal carcinoma. —Thigpen D, et al. [6]
Ultrasound has critics. “Screening [with] ultrasound may lead to unnecessary biopsies,” according to Brian Sprague, assistant professor of surgery at the University of Vermont. “There is a small chance it could save your life, but there is a much greater chance you will have a false-positive result.” Sprague favors tomosynthesis for women with dense breasts. [7]
Tomosynthesis vs. Mammography
Tomosynthesis obtains multiple mammographic images while the x-ray source travels in an arc over compressed breasts, allowing three-dimensional digital breast reconstruction, visualization, and diagnosis. In 2011, the FDA approved digital breast tomosynthesis for all clinical indications accepted for mammography, including screening. [2,8]
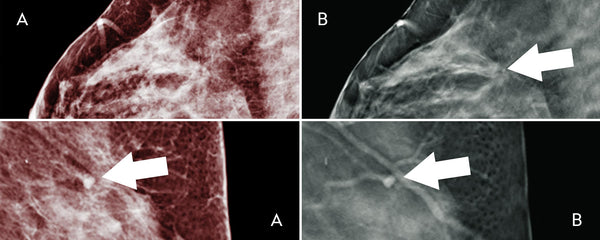
(A) Mammogram captures an asymmetry in the left superior breast. (B) Single tomosynthesis slice demonstrates that the asymmetry is due to a normal vascular structure (white arrow). —Miller JC, D.Phil. [8]
Women between the ages of 40 to 44 should have the option to start annual breast cancer screening with mammograms. According to the American Cancer Society, women age 45 to 54 should get mammograms every year. Women 55 and older should switch to mammograms every 2 years, or may continue yearly screening. [9]
Breast Cancer Drugs May Severely Inflame Lungs
⚠️ October 2019 – The FDA warns that the commonly prescribed breast cancer therapies known as cyclin-dependent kinase 4/6 (CDK 4/6) inhibitors may cause rare but severe inflammation of the lungs.
Healthcare professionals are advised to monitor patients on these drugs regularly for pulmonary symptoms indicative of interstitial lung disease (ILD) and/or pneumonitis, such as hypoxia, cough, dyspnea, or interstitial infiltrates on radiologic exams in patients. —Medscape
![]() As a patient, do you know whether you have dense breasts?
As a patient, do you know whether you have dense breasts?
You cannot feel density. Only a mammogram reveals if patients have dense breasts. Therefore, most ladies are unaware of the diagnosis until they reach the age of 45, when mammograms are recommended or unless there is a family history that warrants earlier testing.
Because mammography equipment is more accessible and it identifies dense breasts, other imaging technologies, like ultrasound, are ancillary, rather than primary diagnostic tools. Tomosynthesis, if available, has FDA approval for screening. [8‑12] Look for the FDA MQSA Certificate at your facility. [13]
FDA MQSA Certificate
To support the writing of scholarly articles about women, ClinicalPosters sells human anatomy charts, scientific posters, and other products online. You may sponsor specific articles or remit a small donation.
ClinicalPosters sells human anatomy charts, scientific posters, and other products online to offset expense of the writing useful articles about women. Slide extra posters into DeuPair Frames without removing from the wall.
Show your support by donating, shopping for ClinicalPins, or leaving an encouraging comment to keep the research going.
To support the writing of useful articles about women, ClinicalPosters sells human anatomy charts, scientific posters, and other products online. You may sponsor specific articles or remit a small donation.
ClinicalPosters sells human anatomy charts, scientific posters, and other products online to offset expense of the writing useful articles about women. Slide extra posters into DeuPair Frames without removing from the wall.
ClinicalPosters sells human anatomy charts, scientific posters, and other products online. You may remit a small donation.
You can support the writing of useful articles about women by sponsoring specific articles or remitting a small donation. Visible content is optimized for device size.






 Romance & Health Intertwine. Fall in love with a captivating romance miniseries that explores the essence of well-being. Become a ClinicalNovellas library member for heartwarming tales.
Romance & Health Intertwine. Fall in love with a captivating romance miniseries that explores the essence of well-being. Become a ClinicalNovellas library member for heartwarming tales.